
Photocoagulation for diabetic macular edema. 2008 145:894–901.Įarly Treatment Diabetic Retinopathy Study Research Group. Retinal thickness on stratus optical coherence tomography in people with diabetes and minimal or no diabetic retinopathy.

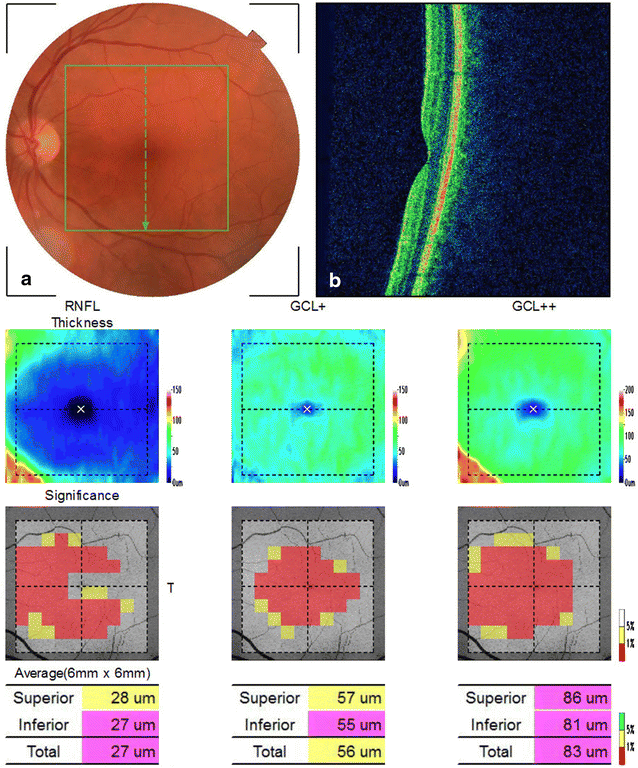
Diabetic Retinopathy Clinical Research Network. 2019 126:1675–84.īressler NM, Edwards AR, Antoszyk AN, Beck RW, Browning DJ, Ciardella AP, et al. OCT angiography metrics predict progression of diabetic retinopathy and development of diabetic macular edema. Sun Z, Tang F, Wong R, Lok J, Szeto SKH, Chan JCK, et al. Multimodal testing reveals subclinical neurovascular dysfunction in prediabetes, challenging the diagnostic threshold of diabetes. Kirthi V, Reed KI, Alattar K, Zuckerman BP, Bunce C, Nderitu P, et al. Foveal avascular zone area and parafoveal vessel density measurements in different stages of diabetic retinopathy by optical coherence tomography angiography. Mastropasqua R, Toto L, Mastropasqua A, Aloia R, De Nicola C, Mattei PA, et al. Enlargement of foveal avascular zone in diabetic eyes evaluated by en face optical coherence tomography angiography. Takase N, Nozaki M, Kato A, Ozeki H, Yoshida M, Ogura Y, et al. Quantitative retinal optical coherence tomography angiography in patients with diabetes without diabetic retinopathy. 2015 35:2364–70.ĭimitrova G, Chihara E, Takahashi H, Amano H, Okazaki K. Detection of microvascular changes in eyes of patients with diabetes but not clinical diabetic retinopathy using optical coherence tomography angiography. 1998 102:783–91.ĭe Carlo TE, Chin AT, Bonini Filho MA, Adhi M, Branchini L, Salz DA, et al. Neural apoptosis in the retina during experimental and human diabetes. OCTA metrics have utility in predicting progression rather than the development of DR in individuals with type 2 diabetes.īarber AJ, Lieth E, Khin SA, Antonetti DA, Buchanan AG, Gardner TW. The area under the receiver operating characteristic curves for VD was AUC = 0.643, with 77.4% sensitivity and 41.8% specificity for a cut-off of 15.85 mm/mm 2 and for MP it was AUC = 0.635, with 77.4% sensitivity and 25.5% specificity for a cut-off of 40.8%. Progression of DR was inversely related to VD ((hazard ratio = 0.825) and to MP (HR = 0.936). Of the 45 eyes with non-proliferative DR (NPDR) at baseline, 17 (37.7%) showed DR progression. 27 of the 161 eyes (16.7%) with no DR at baseline developed new DR, which was associated with a higher baseline HbA 1c and longer diabetes duration. ResultsĪfter four years, 206 eyes of 219 participants were eligible for analysis. OCT-derived macular thickness measures, retinal nerve fibre layer and ganglion cell-inner plexiform layer thickness and OCTA-derived foveal avascular zone area, perimeter, circularity, vessel density (VD) and macular perfusion (MP) were examined in relation to the development and worsening of DR over four years. MethodsĢ80 participants with type 2 diabetes underwent ultra-wide field fundus photography, OCT and OCTA. To assess if optical coherence tomography (OCT) and OCT angiography (OCTA) measures are associated with the development and worsening of diabetic retinopathy (DR) over four years.


 0 kommentar(er)
0 kommentar(er)
